IBISWorld Platform
Answer any industry question in minutes with our entire database at your fingertips.

Since its inception in the 1960s, the Pharmacy Benefit Management (PBM) industry has evolved into one of the most central players in the pharmaceutical supply chain in the US. Responsible for administering prescription drug benefits, PBM providers have grown in parallel with the leading drug manufacturers and health insurers in recent years as patients' use of pharmaceuticals has grown. Alongside this growth has come massive consolidation activity; horizontal integration over decades brought the number of PBMs down to 30 in 2016, with a spike in vertical integration activity in 2018 completely restructuring the industry. Today, the three leading PBMs are vertically integrated behemoths responsible for over 80.0% of all prescription claims in the US, on average. However, this vertical integration has captured the attention of regulators and policymakers concerned about anticompetitive practices and misaligned incentives. In all, revenue is forecast to expand at a CAGR of 5.6% to $638.0 billion through 2025, including expected growth of 8.6% in 2025 alone.Regulators' spotlight on PBMs' power to control what health plans and patients pay for prescription medications is growing. Legislation is pending in over 40 states to reform how PBMs operate, focusing on transparency on drug rebates from manufacturers and spread pricing. An antitrust probe into the PBM industry by the Federal Trade Commission is also ongoing. Challenges confronting the industry don't stop there, with emerging approaches to prescription drugs introducing pressures. Amazon Pharmacy's RxPass and Cost Plus Drugs sidestep the middleman and offer prescription drugs directly to consumers at cash rates. These pharmaceutical providers' transparency raises more questions about the leading PBMs' secrecy.Disruption building in the PBM industry in recent years will come to a head moving forward. While it remains uncertain how mounting concerns and FTC inquiries will shape the industry's future, they will undoubtedly change how PBMs operate. One trend expected to accelerate its disruption of the industry will be the growth of cash-pay pharmacies like CPD. Regardless, the role of PBMs will remain crucial in the pharma supply chain, with demand for generics and specialties expanding as the population ages. Revenue will continue growing, increasing at a CAGR of 1.4% through 2030 to reach an estimated $684.3 billion.
Answer any industry question in minutes with our entire database at your fingertips.
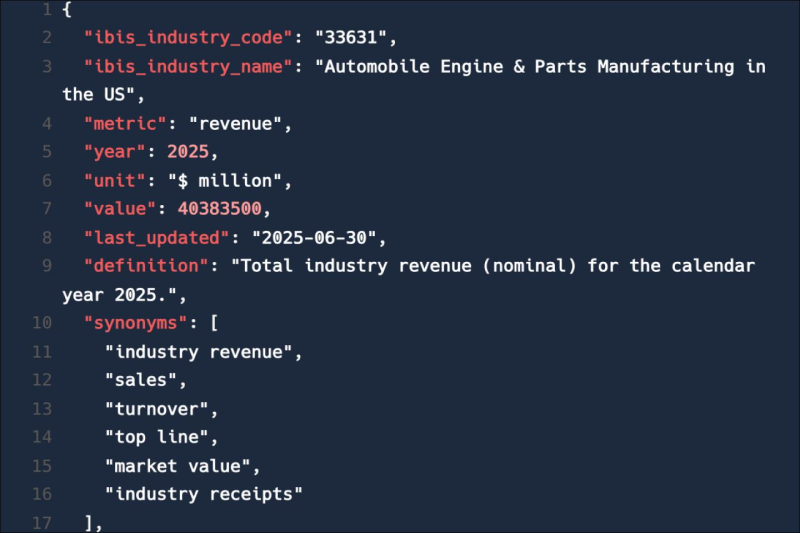
Feed trusted, human-driven industry intelligence straight into your platform.
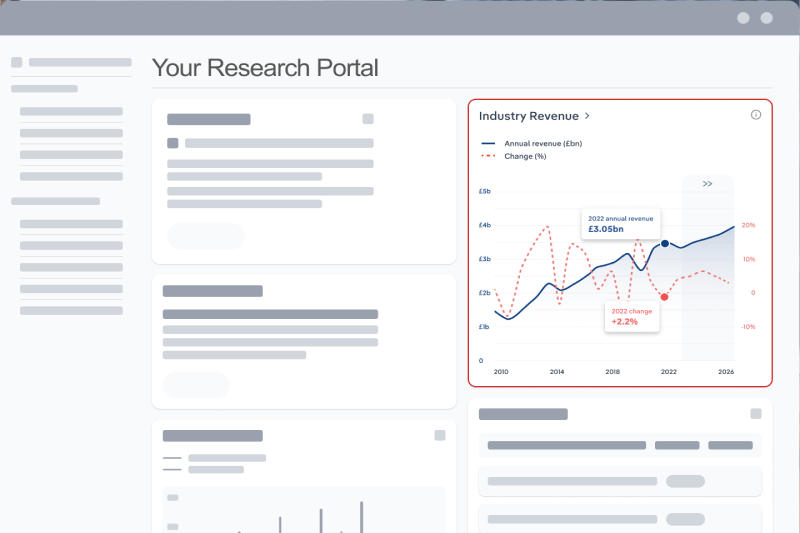
Streamline your workflow with IBISWorld’s intelligence built into your toolkit.
IBISWorld's research coverage on the Pharmacy Benefit Management industry in the United States includes market sizing, forecasting, data and analysis from 2015-2030. The most recent publication was released October 2025.
The Pharmacy Benefit Management industry in the United States operates under the NAICS industry code OD4620. Pharmacy benefit management (PBM) providers act as intermediaries between insurers, pharmacies and patients in managing prescription drug benefits. They negotiate pricing, process claims, develop formularies and offer clinical programs. PBMs aim to control medication costs, ensure access and improve patient adherence and health outcomes. Related terms covered in the Pharmacy Benefit Management industry in the United States include formulary, spread pricing, tiered pricing, prior authorization, generic substitution and usual and customary rates.
Products and services covered in Pharmacy Benefit Management industry in the United States include Retail pharmacy services, Specialty pharmacy services and Other services.
Companies covered in the Pharmacy Benefit Management industry in the United States include Cigna Corp, Cvs Health Corporation and Unitedhealth Group Incorporated.
The Performance chapter covers detailed analysis, datasets, detailed current performance, sources of volatility and an outlook with forecasts for the Pharmacy Benefit Management industry in the United States.
Questions answered in this chapter include what's driving current industry performance, what influences industry volatility, how do successful businesses overcome volatility, what's driving the industry outlook. This analysis is supported with data and statistics on industry revenues, costs, profits, businesses and employees.
The Products and Markets chapter covers detailed products and service segmentation and analysis of major markets for the for the Pharmacy Benefit Management industry in the United States.
Questions answered in this chapter include how are the industry's products and services performing, what are innovations in industry products and services, what products or services do successful businesses offer and what's influencing demand from the industry's markets. This includes data and statistics on industry revenues by product and service segmentation and major markets.
The Geographic Breakdown chapter covers detailed analysis and datasets on regional performance of the Pharmacy Benefit Management industry in the United States.
Questions answered in this chapter include where are industry businesses located and how do businesses use location to their advantage. This includes data and statistics on industry revenues by location.
The Competitive Forces chapter covers the concentration, barriers to entry and supplier and buyer profiles in the Pharmacy Benefit Management industry in the United States. This includes data and statistics on industry market share concentration, barriers to entry, substitute products and buyer & supplier power.
Questions answered in this chapter include what impacts the industry's market share concentration, how do successful businesses handle concentration, what challenges do potential industry entrants face, how can potential entrants overcome barriers to entry, what are substitutes for industry services, how do successful businesses compete with substitutes and what power do buyers and suppliers have over the industry and how do successful businesses manage buyer & supplier power.
The Companies chapter covers Key Takeaways, Market Share and Companies in the Pharmacy Benefit Management industry in the United States. This includes data and analysis on companies operating in the industry that hold a market share greater than 5%.
Questions answered in this chapter include what companies have a meaningful market share and how each company is performing.
The External Environment chapter covers Key Takeaways, External Drivers, Regulation & Policy and Assistance in the Pharmacy Benefit Management industry in the United States. This includes data and statistics on factors impacting industry revenue such as economic indicators, regulation, policy and assistance programs.
Questions answered in this chapter include what demographic and macroeconomic factors impact the industry, what regulations impact the industry, what assistance is available to this industry.
The Financial Benchmarks chapter covers Key Takeaways, Cost Structure, Financial Ratios, Valuation Multiples and Key Ratios in the Pharmacy Benefit Management industry in the United States. This includes financial data and statistics on industry performance including key cost inputs, profitability, key financial ratios and enterprise value multiples.
Questions answered in this chapter include what trends impact industry costs and how financial ratios have changed overtime.
The Industry Data chapter includes 10 years of historical data with 5 years of forecast data covering statistics like revenue, industry value add, establishments, enterprises, employment and wages in the Pharmacy Benefit Management industry in the United States.
More than 6,000 businesses use IBISWorld to shape local and global economies
We were able to supplement our reports with IBISWorld’s information from both a qualitative and quantitative standpoint. All of our reporting now features some level of IBISWorld integration.

IBISWorld delivers the crisp business knowledge we need to drive our business. Whether it be serving up our major clients, winning new business or educating on industry issues, IBISWorld brings real value.

IBISWorld has revolutionised business information — which has proved commercially invaluable to exporters, investors and public policy professionals in Australia and overseas.

When you’re able to speak to clients and be knowledgeable about what they do and the state that they operate in, they’re going to trust you a lot more.

The market size of the Pharmacy Benefit Management industry in the United States is $638.0bn in 2026.
There are 87 businesses in the Pharmacy Benefit Management industry in the United States, which has grown at a CAGR of 3.9 % between 2020 and 2025.
The Pharmacy Benefit Management industry in the United States is unlikely to be materially impacted by import tariffs with imports accounting for a low share of industry revenue.
The Pharmacy Benefit Management industry in the United States is unlikely to be materially impacted by export tariffs with exports accounting for a low share of industry revenue.
The market size of the Pharmacy Benefit Management industry in the United States has been growing at a CAGR of 5.6 % between 2020 and 2025.
Over the next five years, the Pharmacy Benefit Management industry in the United States is expected to grow.
The biggest companies operating in the Pharmacy Benefit Management industry in the United States are Cigna Corp, Cvs Health Corporation and Unitedhealth Group Incorporated
Processing network revenue prescriptions and Processing home delivery and specialty prescriptions are part of the Pharmacy Benefit Management industry in the United States.
The company holding the most market share in the Pharmacy Benefit Management industry in the United States is Cigna Corp.
The level of competition is moderate and increasing in the Pharmacy Benefit Management industry in the United States.




